Why Vaccinated People Are Not Taking Delta Seriously Enough w/ Dr. Eric Topol (The New Abnormal, 13 Aug 2021)
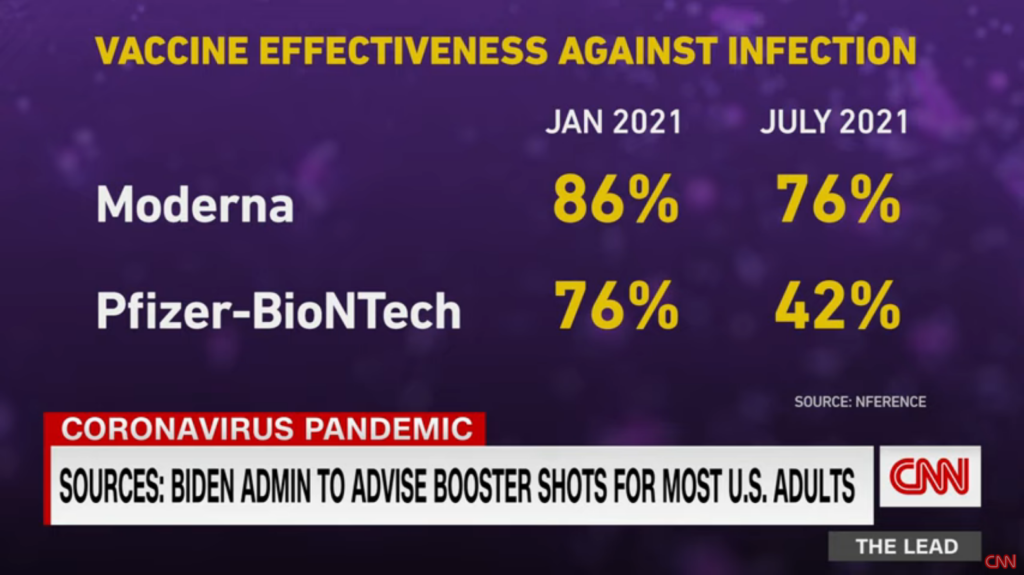
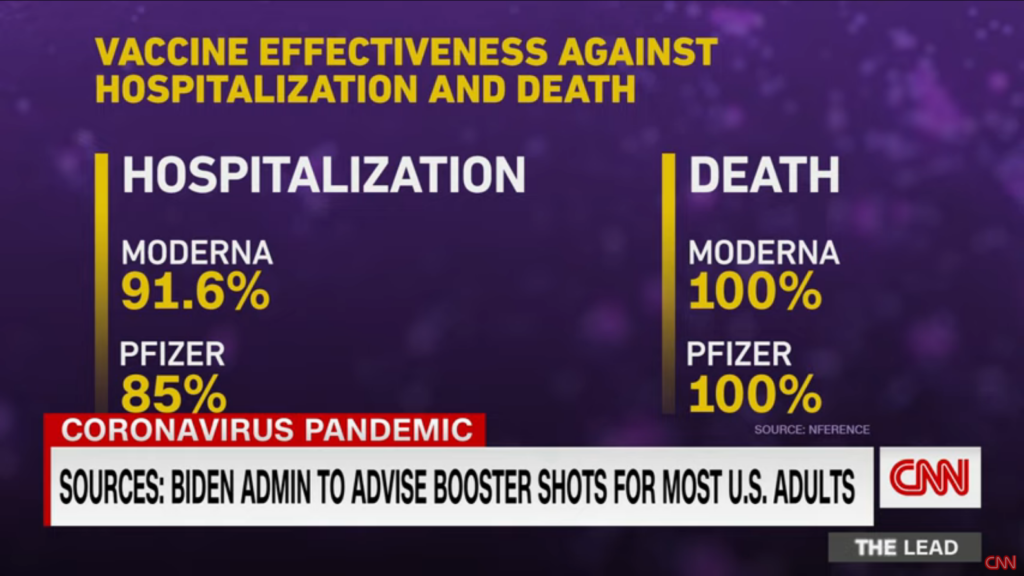
Dr. Eric Topol (good reporting on his Twitter feed) reports that current vaccines provide protection from delta at around 40-60% effectiveness and a booster would bring that to 90%. The data from a CNN report expands/clarifies those numbers but provides no data on boosters (see images below). On 13 Aug 2021, the CDC advised that immunocompromised people start getting boosters and there are reports that the federal government will recommend all others to get one eight months after their previous shot (our 2nd dose of the Pfizer was 11 Apr 2021, so hello Dec 2021).
Should the US be distributing boosters?
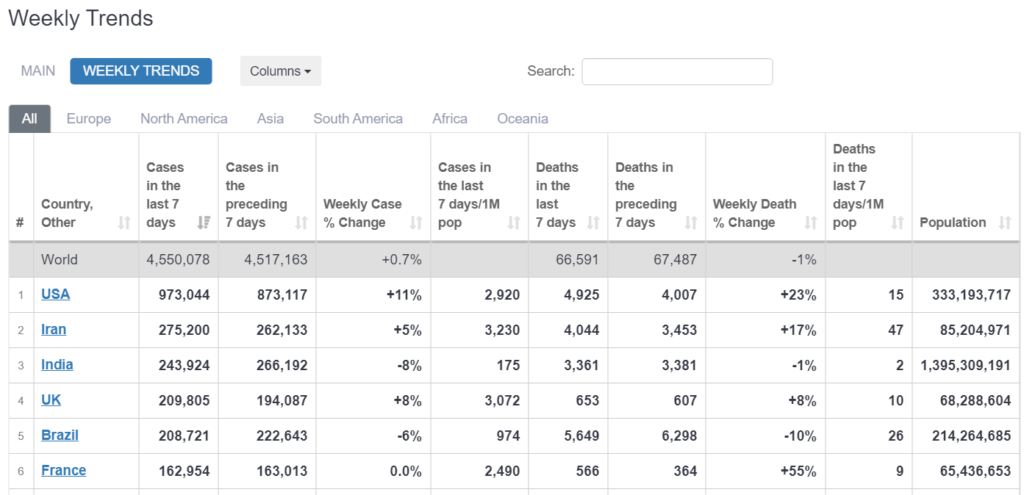
The question is whether we should use our resources towards delivering boosters within the country or instead ship vaccines to countries that have none at all (or a combination). We’ve been throwing away the doses that morons refuse to take so why not provide them to countries that want them? That being said, there has been a strong increase in vaccinations over the past month or so, so there is an increased desire and need here at home. And our numbers are just Not That Good compared to the rest of the world so maybe we’re the ones in need.
What is long-hall COVID?
The CDC labels it simply as post-COVID conditions and lists 18 symptoms. Wikipedia lists 26 symptoms and categorizes it as an idiopathic disease (unknown cause) and a diagnosis of exclusion (one that “tends to occur where scientific knowledge is scarce, specifically where the means to verify a diagnosis by an objective method is absent”). It appears that we just don’t know if these symptoms are caused by understandably long recovery periods (compounding existing conditions) or will be exceptionally long or even lifetime conditions.
CDC continues to work to identify how common post-COVID conditions are, who is most likely to get them, and why some symptoms eventually resolve for some people and may last longer for other people. Rapid and multi-year studies are underway to further investigate post-COVID conditions.
from Post-COVID Conditions at the CDC, last updated 12 Jul 2021
Is ICU capacity meaningful?
The answer is likely that there is not a strict numeric correlation over time between capacity and the ability to provide care.
Fact check: Hospitals staff near max capacity, but COVID-19 isn’t business as usual (USA Today, 9 Aug 2021)
ICU Bed Capacity Varies Widely Nationwide (NPR, 25 Mar 2020)
Noting the range of dates for the articles above, this has been a constant debate. The key takeaway is that doctors and nurses available for ICU beds may be able to handle patients healing from gunshot wounds or car-crashes with more capability than those patients with COVID.
While I may be able to count the number of beds in Region A and Region B and the underlying populations in those two areas, what those beds and ICUs are actually able to provide is an entirely different question.
David Wallace, quoted in the NPR article from 2020
There’s still a lot of new information to parse and I’m getting tired of this shit.
Acquired two new movie posters as an aesthetic balm: